There are many myths surrounding the management of Osteoarthritis (OA), especially when it comes to exercise. Some common misconceptions include “weight-bearing exercises are bad for my joint health”, “surgery is the only option to improve my OA”, or “movement will make my OA worse – I should just rest”. However, the fact is, appropriately prescribed physical activity is recommended and effective in improving your OA symptoms, and a lack of physical activity has been shown to progress the condition and make symptoms worse.
This article explains Osteoarthritis (OA), and how exercise can help, we cover;
– WHAT EXACTLY IS OSTEOARTHRITIS?
– HOW DOES EXERCISE HELP WITH OA?
– WHAT TYPE OF EXERCISE IS BEST?
– STARTING YOUR EXERCISE ROUTINE
– HELPFUL GUIDELINES ON EXERCISE
What is Osteoarthritis?

Osteoarthritis (OA) is a chronic condition characterised by deterioration of cartilage that overlies the ends of bones in joints. This can occur naturally from years of movement, friction, mechanical pressure over the surfaces, and previous injury to the joint. The most common joints affected by OA are those of the hips, knees, feet, hands, and spine. The most common symptoms associated with OA are joint pain, stiffness, swelling, and tenderness.
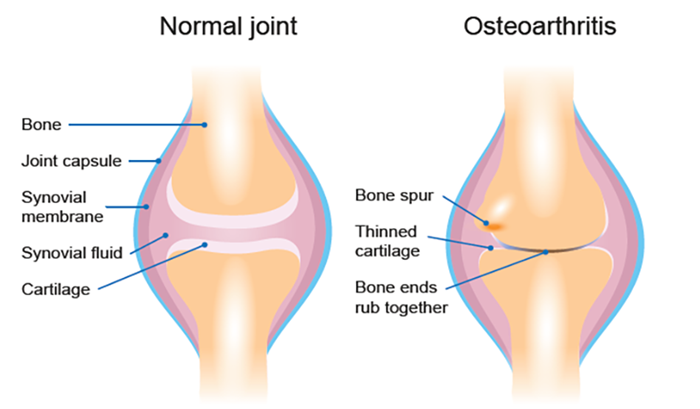
Comparison of healthy joint and joint with osteoarthritis
OA is the most prevalent chronic joint disease in Australia and is the main condition leading to knee and hip replacement surgery in Australia. 1 in 11 Australian’s (9.3%) have OA, approximately 2.2 million people in 2018. More than 1 in 2 Australian’s with OA report moderate to very severe pain.
– How Does Exercise Help with OA?
You may have heard the phrase “exercise is medicine”, and in the cause of hip and knee OA, it holds true. Exercise will not only help to manage symptoms, but it may also help to prevent the bone and joint deterioration associated with OA. Many high-quality studies show that exercise therapy is effective and highly recommended as a conservative management strategy for people living with OA.
Some of these benefits include;
- Reducing joint pain
- Improving joint range of motion and function
- Increasing muscle strength reducing deconditioning.
- Improving balance, coordination, and flexibility.
- Promotion of weight loss (excess body weight contributes to OA complications).
- Improved overall health and well-being.
- Prolong the need for surgical intervention and improve surgery outcome.
As pain and stiffness are the most common symptoms associated with hip and knee OA, it is often accompanied by reduced physical activity levels. Physical inactivity has been linked to reduced cardiorespiratory fitness and obesity, which are high-risk factors for other chronic health conditions such as type 2 diabetes, cardiovascular disease, osteoporosis, and many more. Therefore, it is important to find an activity that is safe and effective, but most importantly, something that is achievable and that you will commit to.
– What Type of Exercise is Best?

A combination of strength (resistance) training, aerobic exercise, balance, and flexibility exercises are recommended for people suffering from OA. This can be achieved through many different types of activities and it is important to find an activity that you enjoy.
- Aerobic exercise: This may include walking, cycling, swimming, rowing, or any sustained activity where your heart rate and breathing are increased. Regular aerobic exercise can help you sleep better, burn calories for weight management and increase your energy levels and general health. Aim to accumulate 150 minutes of moderate-intensity aerobic exercise throughout the week.
- Resistance training: As joint damage and chronic pain can lead to muscle atrophy and weakness, poor balance, and decreased mobility, resistance training forms an essential part of exercise intervention for patients with OA. You can use your own body weight as resistance, or equipment such as dumbbells, resistance bands, and machine weights. Often the muscles of the hip, knee, and ankle joints are weakened for people with OA so should be a focus area. Aim to include some form of resistance training focusing on large muscle groups on at least two non-consecutive days throughout the week.
- Aquatic (water) activities: Exercising in water significantly reduces the load experienced within your joints. People who are overweight or those with severe disease may find aquatic exercise particularly helpful. Water exercise can be a useful starting point before progressing to, or in combination with land-based exercises.
- Other forms of exercise: Activities such as Tai-Chi, Yoga, and Pilates are low impact and have been shown to be beneficial in people living with OA. These activities help to improve joint function through increased strength, range of motion, flexibility, and balance.
– Getting Started

It is important to choose exercises that you enjoy and can be easily incorporated into your lifestyle. You can exercise indoors, at home, outdoors, or in a supervised environment such as a gym or fitness centre. It is important to start out gently and slowly progress your physical activity levels.
General exercise is going to be beneficial for overall health and well-being and will help to improve your OA symptoms. However, as the biomechanics and musculature vary between different segments of the body (e.g., hip and knee joints), it may be beneficial to consult with one of our Accredited Exercise Physiologist’s or Physiotherapist’s to create an individualised exercise program that is right for you.
– Helpful Guidelines on Exercise

- Aim to include some form of physical activity most days of the week.
- You may experience some pain or discomfort during physical activity, this is normal. However, if you experience major increase in pain or swelling it may indicate the need to modify your activity. Consider the FITT principle (frequency, intensity, time, and type – an accredited exercise physiologist or physiotherapist can assist you here).
- Start out slow and progressively build up your physical activity levels; if you start out too hard your symptoms may become aggravated.
- If you are overweight your OA symptoms are generally exacerbated. Consider implementing healthy food choices and portion control in conjunction with your exercise program to improve outcomes.
- If you stop exercising, the benefits you have achieved will reduce over time. Some strategies to improve exercise adherence and motivation can include exercising with a friend, keeping a logbook, setting achievable goals, and keeping your physical activity interesting.
For more information on managing your Osteoarthritis, our team of Exercise Physiologists and Physiotherapists can assist you. We can provide a tailored exercise program to suit your needs and lifestyle, provide support and guide you on how to safely implement exercise into your week. Contact Fluid Physio + Gym for more information on 6646 3766.
Or to book online, simply click here. We are confident we can help you.
For more information on Aaron Pateman visit team bio.
References:
Australian Institute of Health and Welfare 2020. Osteoarthritis. Cat. no. PHE 232. Canberra: AIHW. Viewed 03 December 2020,https://www.aihw.gov.au/reports/chronic-musculoskeletal-conditions/osteoarthritis
Fransen et al (2015) Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med 49:1554-7.
Osteras et al (2017) Exercise for hand osteoarthritis. Cochrane Database of Systematic Reviews, Issue 1. Art. No.: CD010388.
Quicke et al (2015). Is long-term physical activity safe for older adults with knee pain? A systematic review. Osteoarthritis & Cartilage
Fransen et al. (2014) Exercise for osteoarthritis of the hip. Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD007912.
Rausch Osthoff et al (2018) 2018 EULAR recommendations for physical activity in people with inflammatory arthritis and osteoarthritis. Ann Rheum Dis 77:1251-60









About The Author: Aaron Pateman
More posts by Aaron Pateman